Chronic diseases are defined by the CDC as “conditions lasting one year or longer that require ongoing medical attention or limits daily activities, or both.”
Heart disease, stroke, and diabetes are three of the most prevalent diseases burdening Americans today. Heart disease & stroke are responsible for over a third of all total yearly deaths and approximately $214 billion in cost to the healthcare system. Additionally, over 38 million Americans live with diabetes, with another 84 million Americans classified as “pre-diabetic” — another serious health condition where blood sugars lie between normal and diabetic range, but patients are at a higher risk for diabetes, heart disease, and stroke. An additional $237 billion is spent on diabetes-related management annually, but this number can be misleadingly low, as over 90% of people with pre-diabetes go undiagnosed.
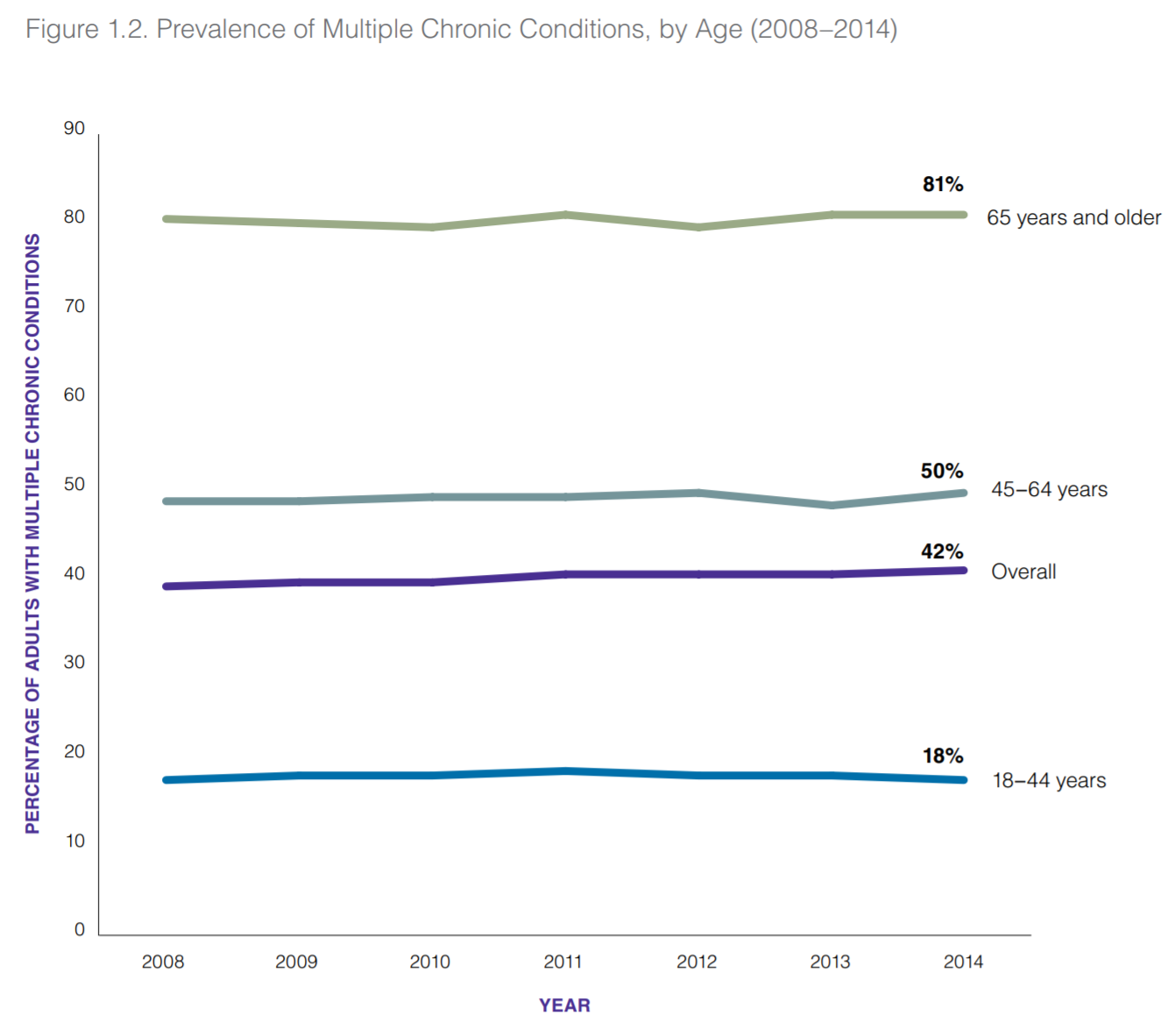
As of today, 60% of the adults in the US have at least one chronic disease, with 40% of adults coping with two or more.
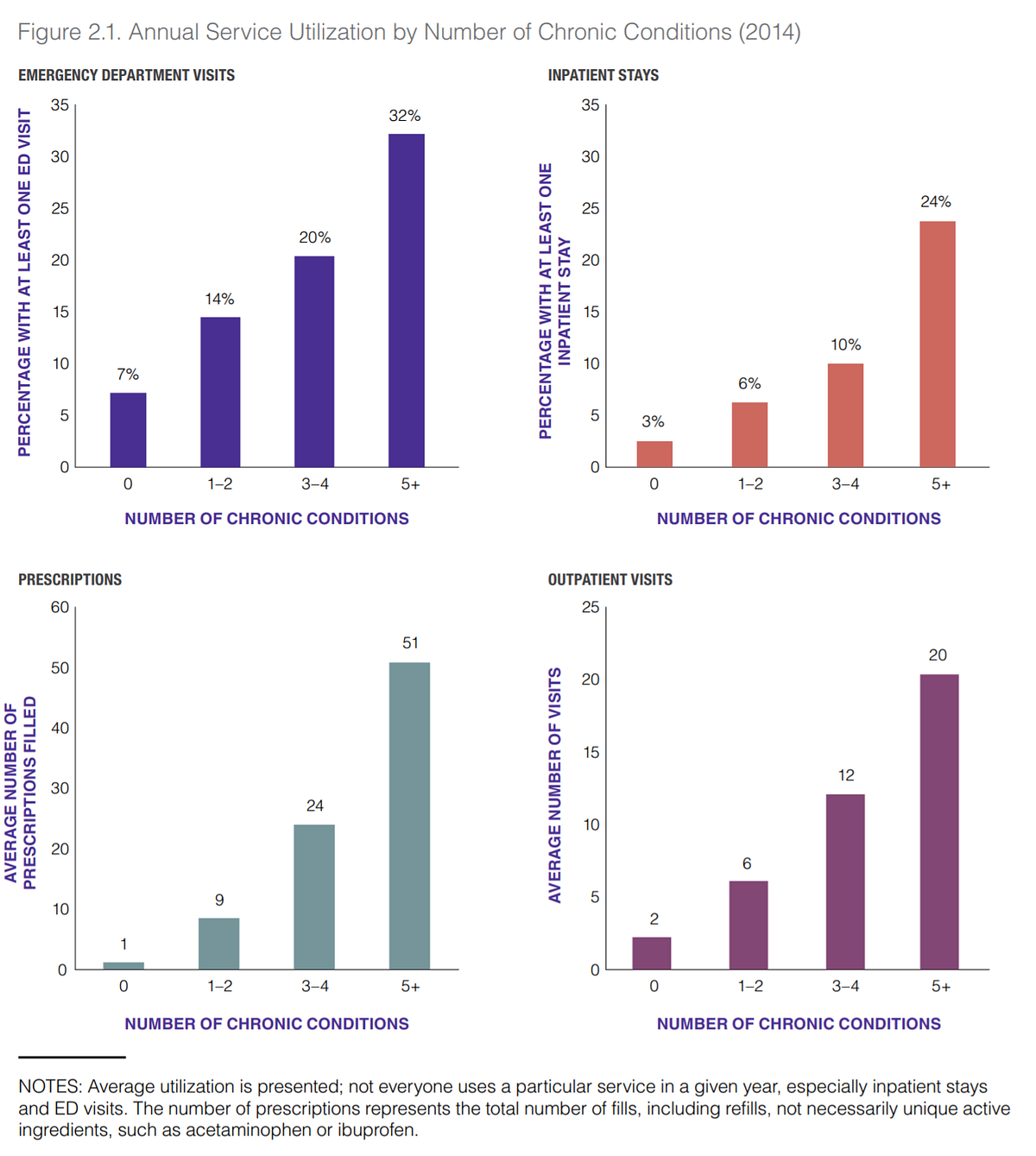
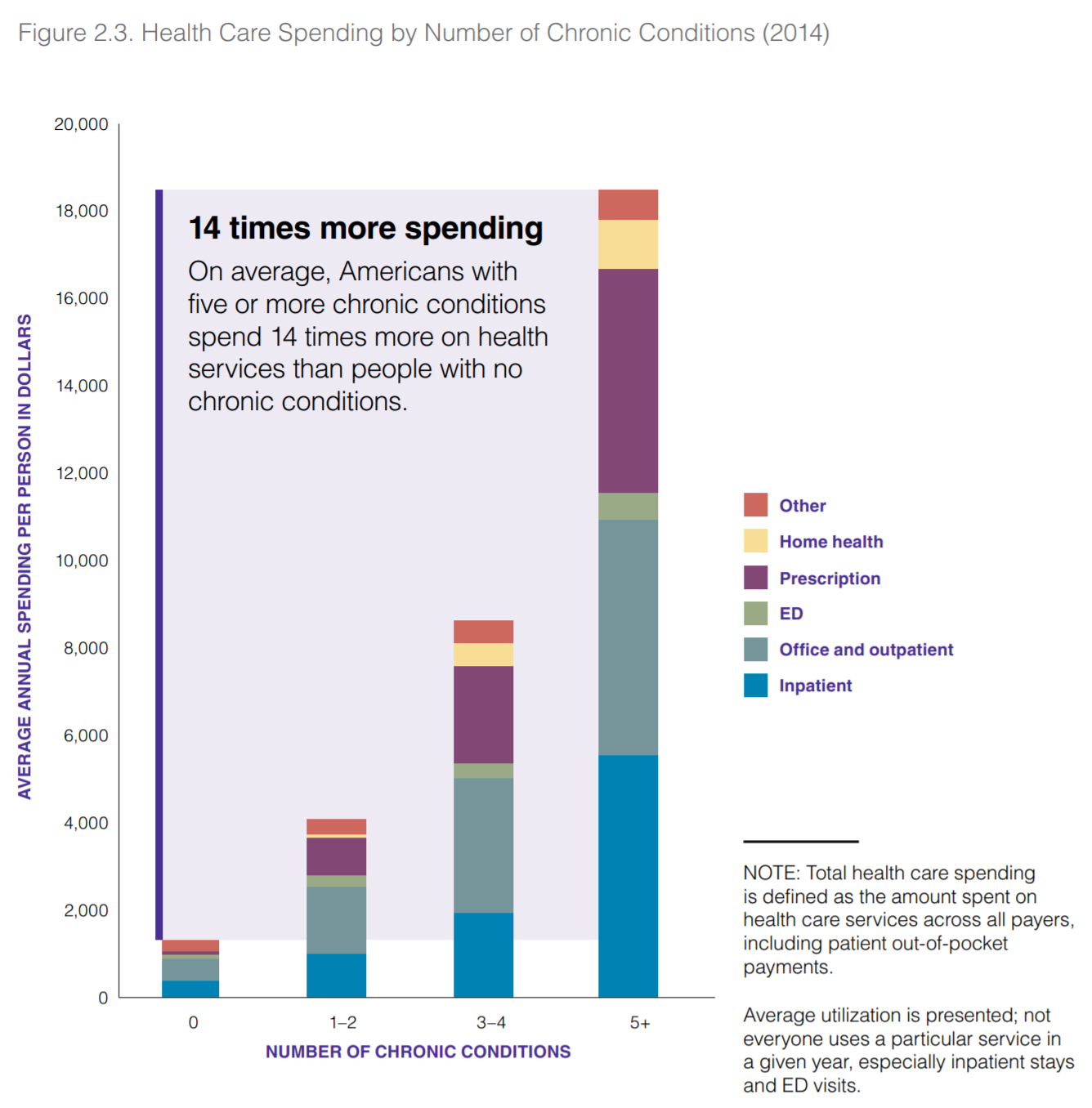
A 2014 review by the RAND Corporation illustrated how patients living with these conditions have increased social and functional limitations, increased hospital visits, more prescribed medications, and higher monetary expenditure — all of which are directly correlated to the number of concurrent chronic diseases an individual has:
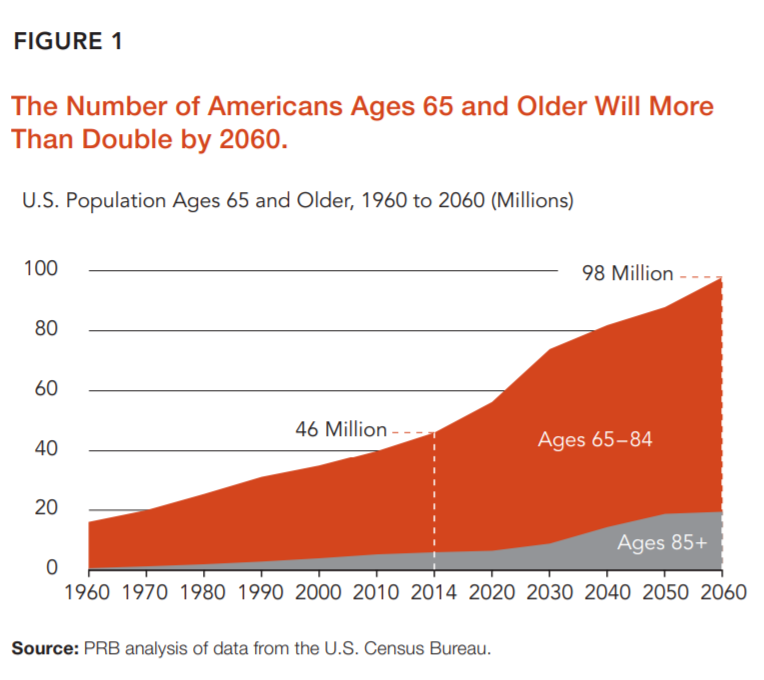
As the prevalence of chronic conditions rises in step with the United States’ increasing median age, it will be crucial to develop and scale efficacious methods to help manage chronic conditions and control their underlying risk factors.
What can we do?
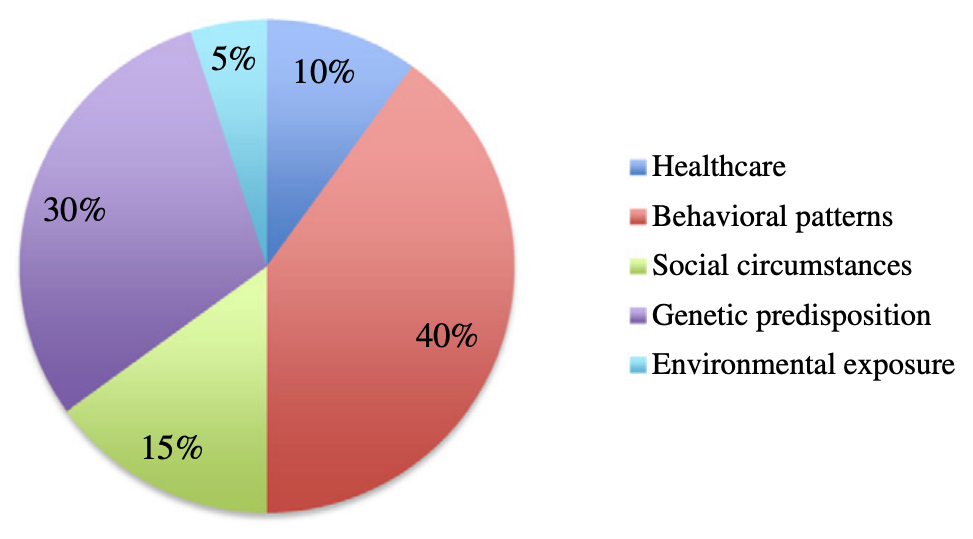
The largest and most critical determinants of health are behavioral patterns such as diet, exercise, patient engagement, patient perception, and medication adherence, which contribute to 40% of an individual’s lifetime health status. To understand behavioral patterns and their association with a unique individual’s health, clear, clean data on specific activities related to a person’s everyday life (and their health) is essential.
Building this holistic picture requires the use of telemedicine, mobile medical software, and wearable hardware to create a framework where health data can be aggregated, analyzed, and successfully interpreted to improve patient outcomes while reducing costs and the probability of medical errors. A portion of this is already happening with the rise of consumer wearables and data-generating physiological and sociological instruments ranging from fitness trackers to smartphone usage:
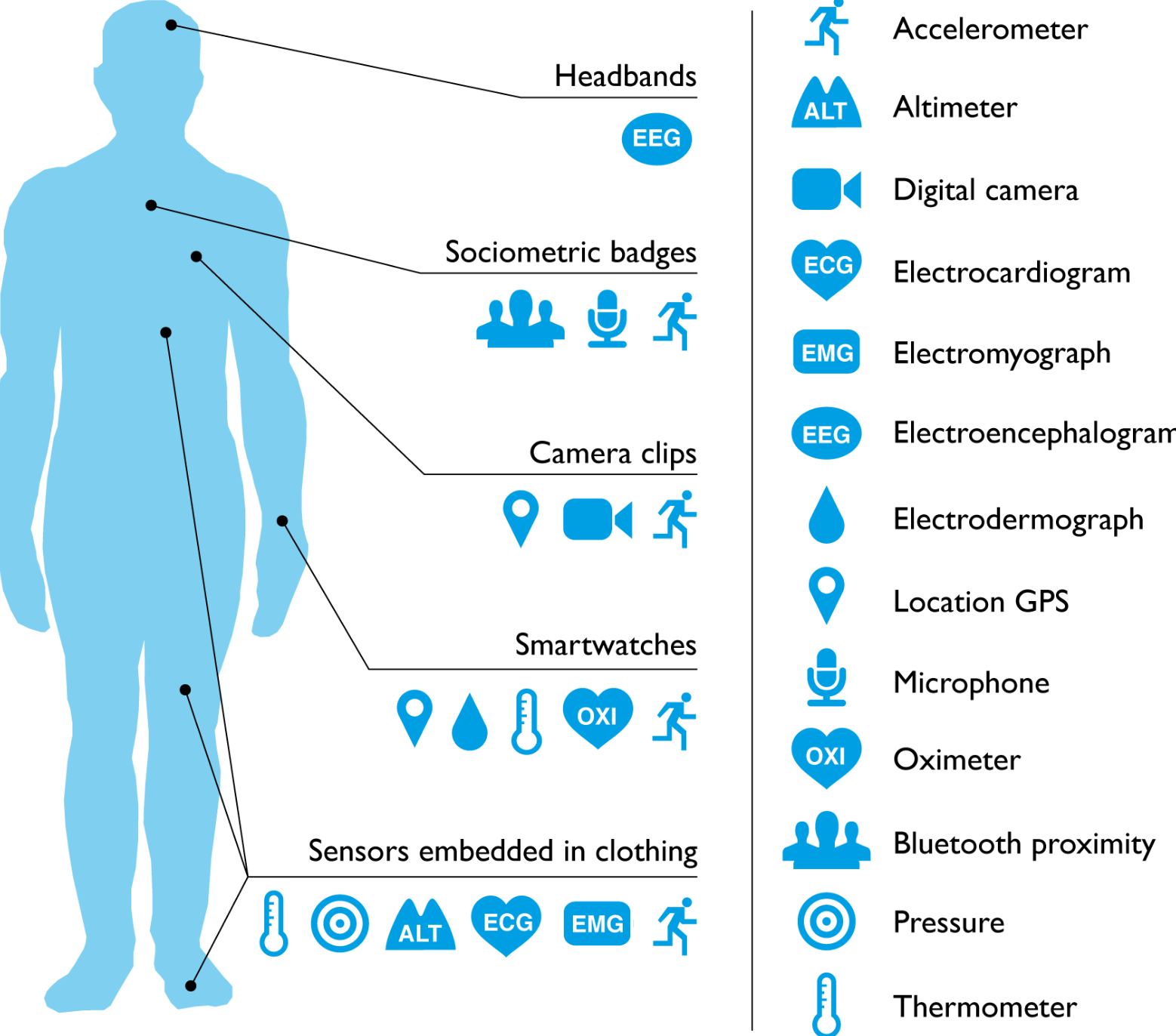
By generating and collecting longitudinal data, clinicians and patients alike are privy to clearer insight into their conditions while also offering instantaneous personalized feedback and interventions. Several studies and reviews through the years have consistently validated the aforementioned benefits supplied by real-time monitoring through digital wearable technology, including HealthTech, HIMSS, AJHP, AHA Journals, and Johns Hopkins Medicine.
These studies show how increased patient engagement through self-monitoring of relevant disease-associated metrics (e.g. BP, glucose, physical activity, etc.) and the use of integrated multidisciplinary care teams (including physicians, nurses, and pharmacists) can empower the patient to take control of their own chronic conditions and help the care team reinforce positive lifestyle choices through shared clinical decision-making.
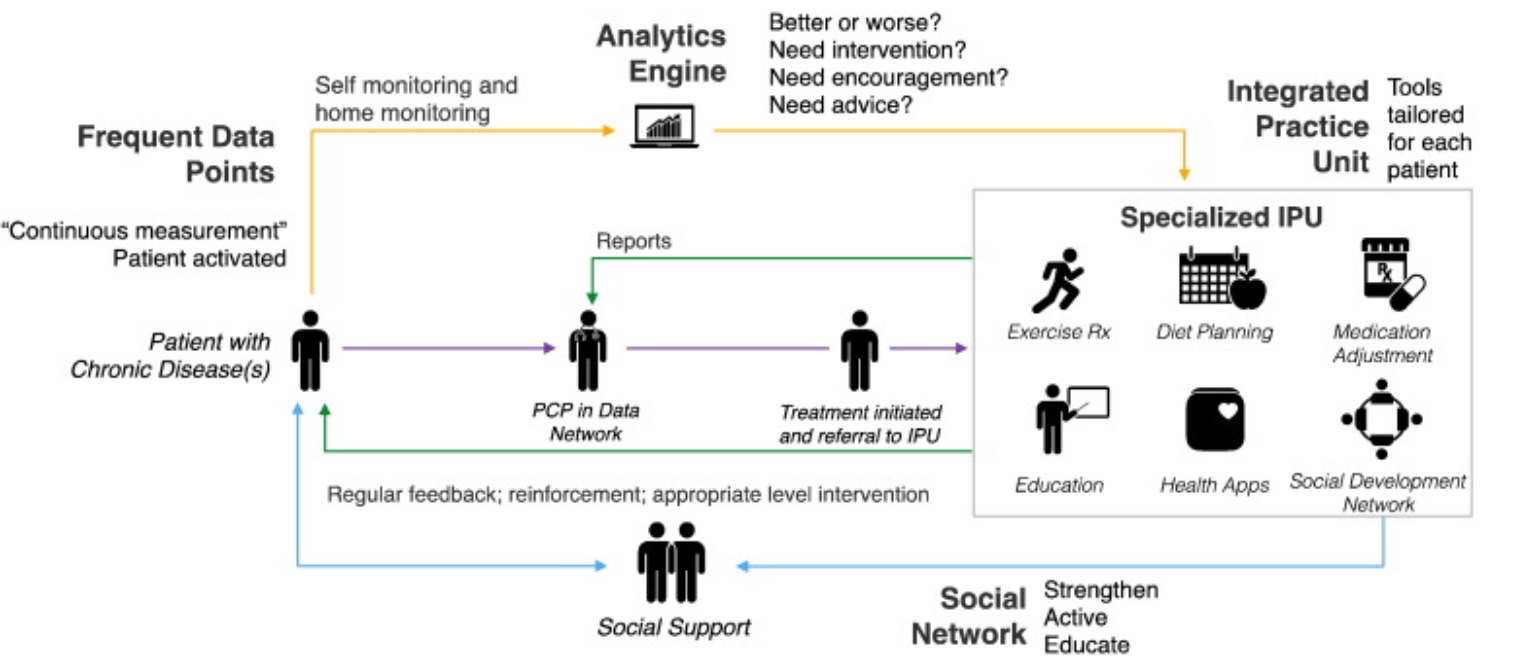
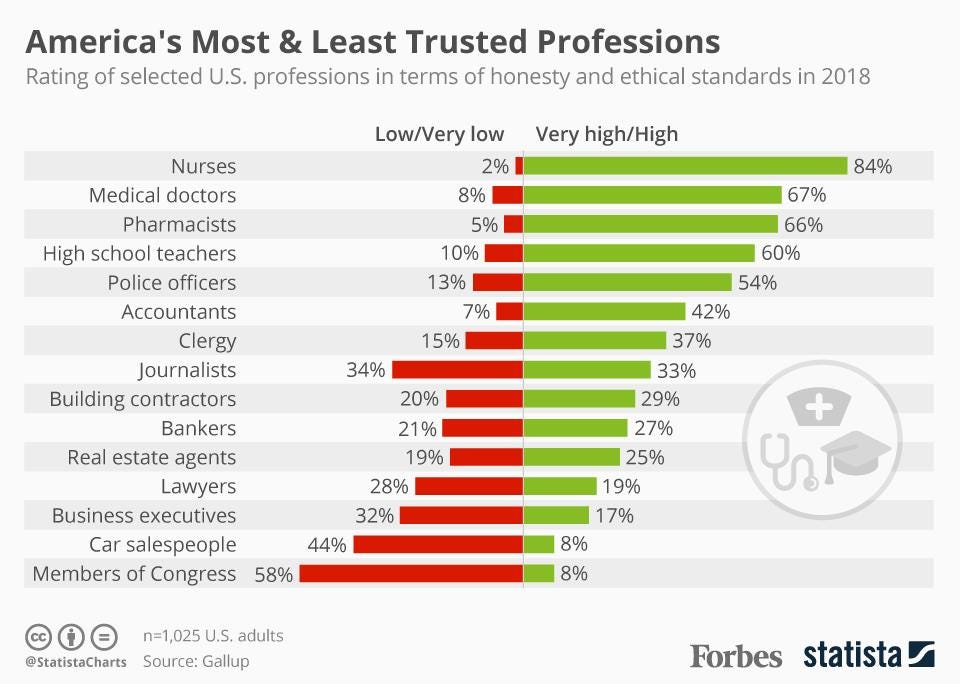
As medication experts, pharmacists occupy a unique — and impactful — role on the front lines of chronic disease management and intervention. Pharmacists are trained in clinical techniques including educating patients to address underlying risks, providing medication regimen management, immunizations, and performing targeted counseling using motivational interviewing techniques. The positive impact clinical pharmacists can have on chronic disease outcomes is extensively documented and is even greater when working in interdisciplinary collaborative settings.
Pharmacists are trained to interpret physiological readings, behavioral information, and medication regimens simultaneously to construct ideal personalized treatment regimens to drive outcomes. In addition to the benefit of patient trust, pharmacists have significantly more opportunities for patient interaction than primary care or specialty providers, as they come into contact with patients with much greater frequency.
With the expansion of longitudinal digital monitoring of clinical and digital biomarkers through wearables and apps, pharmacists are uniquely positioned to provide a distinctive intervention, empowerment, and management strategy to patients with chronic conditions, resulting in vastly improved health outcomes.
Looking into the crystal ball…
Even though wearable device usage is projected to skyrocket with the advent of new technology via major players such as Google, Sony, Apple, and Samsung, several barriers are preventing further proliferation and integration of these digital products into clinical use. These include mistrust in data security/reliability, lack of appropriate digital infrastructure (for data collection, analysis, and integration into Electronic Health Records), patient attrition (due to lack of engagement and/or understanding of technology), lack of healthcare provider recommendations, and negative user experiences with healthcare providers in the digital space.
Increased cooperation between clinical experts (including pharmacists) and product developers can bridge gaps in understanding what data is required of these devices to make sound medical decisions, and what is currently feasible. With this greater understanding, targeted patient protocols can be formed and workflows for device functionality and measurement of impact on overall patient health can be implemented and standardized to involve patients across various demographics and an expanding list of disease states. What remains crucial is the interpretation and actionability of the data received, as the outputs must provide both context and clinically valid recommendations to be 1) Trusted, 2) Used Widely, and 3) Accepted as part of a clinical workflow.
Additionally, AI and Machine Learning are being used today to help analyze & interpret the large amounts of raw data coming from these assorted digital devices to improve health intervention and management strategies through algorithms that can learn from (and prompt clinicians and patients to act on) incoming metrics in real-time.
The potential for digital devices/wearables — especially in the management of chronic diseases — cannot be understated. The valuable health data they provide will be critical to the scaled provision of personalized individual care, the shaping of public health policy related to chronic disease, and the ability to improve key clinical and behavioral outcomes related to patient health.
Pharmacists who can leverage these datasets via intelligent systems will play a key role in ensuring chronic disease patients live longer and better.
Tags:
Blog Posts
May 24, 2021




Comments