Medication-related problems (MRPs) are issues caused by prescription medications that can interfere with a patient’s health or therapy goals.
Older adults, in particular, are more at risk for MRPs. Medications prescribed to older adults represent 33% of all medications prescribed. The average older adult takes eight medications daily. This phenomenon, called polypharmacy, puts older adults at higher risk of experiencing problems such as treatment failure or adverse drug reactions.
The high costs to patients and healthcare organizations
The costs of medication-related problems are staggering. They have become a leading cause of death in the U.S., and up to 750 older adults are hospitalized per day for issues related to non-optimized medications. They are also a leading cause of avoidable hospital admissions and emergency department visits, reducing quality of life and diverting valuable dollars to avoidable healthcare costs.
Assessing the financial toll
MRPs carry a heavy financial toll on plans, providers, and patients. In the United States, the total cost of non-optimized medications and subsequent medication problems was estimated at $528 billion in 2016, or 16% of all U.S. healthcare system expenditures.
The toll on patient health
Medication-related problems do more than hurt wallets. Patients feel the effects physically as much as financially, experiencing more health problems, taking more trips to the hospital, and struggling to achieve their health goals.
Older people, in particular, because of their age, experience more health problems and chronic medical conditions, resulting in more visits to the doctor. Care for chronic conditions is often pushed out to specialty healthcare professionals who provide care in silos. In this fractured, uncoordinated care delivery system, patients are at increased risk of medication errors. As a result, patients with chronic conditions, like congestive heart failure (CHF), hypertension, or dementia are more affected by medication-related problems, including drug-drug interactions, drug-disease interactions, ineffective drug therapy, or reduced quality of life. One study found that 93% of patients with dementia had at least one MRP like falls with injury or drug toxicity and higher health care costs.
Even when the right medications in the right dose are prescribed for the right reasons, medication-related problems are prevalent in the older population. The sheer volume of pills ingested daily can create confusion and errors on the part of the patient. Coordinating refills for eight or more medications (often across multiple pharmacies) can be challenging and result in medication-related problems and adherence issues. In a 2019 study published in the Journal of Managed Care and Specialty Pharmacy, researchers found that Medicare Part D beneficiaries taking more than 11 medications were twice as likely to experience drug-related problems as those taking fewer medications, potentially causing unnecessary hospitalizations and costly emergency department visits.
7 reasons for medication-related problems
Solving the costs of medication-related problems starts with understanding why they happen in the first place.
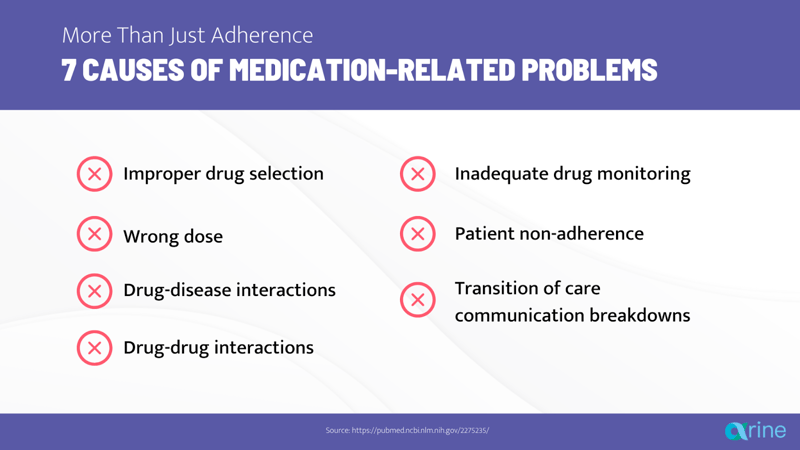
1. Inappropriate drug selection
Inappropriate medication selection happens when a patient is not on the best medication to treat their health conditions. It also occurs when the medication prescribed isn’t optimal based on their age, other disease states they may have, and other medications they may take. Inappropriate drug selection happens in two main ways:
Underprescribing
In underprescribing, providers fail to prescribe medications to patients who need them. For example, laxatives may be underprescribed to a patient taking opioids. Or angiotensin-converting enzyme inhibitors (ACEIs) can be underprescribed in patients with CHF.
Overprescribing
In overprescribing, patients may be taking a medication when it is not indicated. For example, perhaps the medication was originally intended to treat an acute condition, but the prescription was never stopped when the condition was resolved. Or, in other cases, a provider may prescribe a medication to treat the side effects of another medication instead of managing that side effect by optimizing or discontinuing the first medication.
2. Wrong dose
Even when patients take the correct medications, their doses may not be optimized, which leads to treatment failure.
For example, in a study published in the Joint Commission Journal on Quality and Patient Safety, fewer than half of the patients in the study, about 45%, were prescribed the appropriate doses of therapies for heart failure. Most patients were underdosed, despite the well-established fact that medication titration in heart failure can reduce mortality, reduce heart failure hospitalizations, and improve quality of life.
One study in the Journal of American College of Cardiology looked at patients on direct oral anticoagulants (DOACs) for stroke prevention. Almost half of patients with renal impairment were potentially overdosed, putting them at a higher risk of bleeding. Another 10% of patients with normal renal function were underdosed, increasing their risk of stroke.
3. Drug-disease interactions
For some patients, medication-related problems are caused by interactions between their disease states and the medications they take. Examples of serious drug-disease interactions that can cause MRPs inelderly patients include the following:
- Use of first-generation calcium channel blockers in patients with CHF.> These can worsen CHF.
- Use of aspirin in patients with peptic ulcer disease. Aspirin can increase the risk of gastrointestinal bleeds
- Use of antipsychotics in patients with Parkinson’s disease. These can worsen the symptoms of the disease.
- Use of thiazide diuretics in patients with gout, which can exacerbate gout symptoms
- Use of non-steroidal anti-inflammatory drugs (NSAIDs) in patients with kidney disease, which can cause kidney injury.
4. Drug-drug interactions
Another common cause of medication-related problems is drug-drug interactions. Like drug-disease interactions, drug-drug interactions are more common in older adults due to age-related physiological changes, higher incidence of multiple disease states, and medication use. As a result, drug-drug interactions put older adults at an elevated risk of hospitalization. Examples of medication-related problems due to drug-drug interactions include the following:
- Renal injury caused by ACEIs and sulfamethoxazole/trimethoprim.
- Hyperkalemia caused by concurrent drug use of ACEIs and potassium-sparing diuretics.
- Increased risk of bleeding due to warfarin interacting with antibiotics, like azithromycin.
- Altered mental status when benzodiazepines or zolpidem are used concomitantly with opioids.
- Patients consuming over-the-counter (OTC) drugs that interact with their prescription drugs.
5. Inadequate drug monitoring
Drug monitoring includes monitoring the achievement of the goals of therapy (controlled blood pressure, controlled blood sugar), checking for adverse effects of the therapy, performing necessary lab tests to check the efficacy of the therapy (lipid tests, metabolic panels, drug levels), and regularly re-assessing the need for medication.
When patients receive inadequate monitoring, they could experience therapeutic inertia and MRPs like adverse drug events, drug-drug interaction, and therapy failure.
6. Lack of patient adherence
Patient non-adherence is often cited as the main reason for medication-related problems.
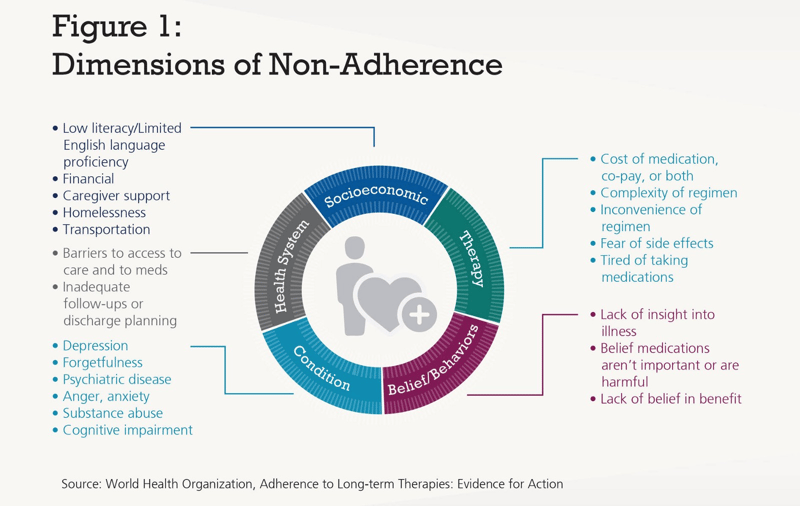
According to the World Health Organization, medication adherence in people with chronic diseases averages 50% in developed countries. Low adherence can be due to different factors:
- Socioeconomic factors like patient education, social support, or financial status. For example, depending on their health literacy, patients may not feel the need to take medications because they don’t understand why their medications are necessary, or they may stop taking their medications or skip months because they can’t afford to pay for them.
- Therapy-related factors such as side effects of the medication and therapy complexity. A patient may be less adherent to a complex drug regimen that has to be taken several times a day, or with specific meals.
- Patient-related factors like patient age, beliefs, or preferences. Geriatric patients may experience memory problems and not take their medications as directed.
- Condition-related factors—are they showing symptoms or not? Patients may or may not feel the need to take their medications if their condition is symptomatic or not. For instance, they may only take their scheduled blood pressure medication as needed when they “feel” that their blood pressure is high.
But, medication adherence is not the only factor that causes medication-related problems. If medications aren’t indicated, effective, or safe for a patient, asking them to adhere can be dangerous or even deadly.
7. Poor communication and breakdown at the transition of care
MRPs also result from communication breakdowns as the older adult transitions from one care team to another.
Miscommunication and misunderstanding during doctors' appointments
In the doctor’s office, providers may not educate patients properly on their conditions and therapies, patients may mishear or forget, they may not comprehend the information they are provided, or they may have language barriers preventing them from understanding instructions.
At the pharmacy
At the pharmacy, patients may not receive counseling from their pharmacists due to the busy environment of retail pharmacies. Additionally, patients may also see different providers and fill their prescriptions at different pharmacies, with each provider or pharmacy unaware of the other, leading to duplication of medication therapy.
During hospital admission
Mistakes can be made during the medication reconciliation process when a patient is admitted to the hospital. This can lead patients to continue taking medications that they were supposed to stop or miss medications they’re supposed to be on during their admission.
At hospital discharge
Patients and caregivers may not be educated properly on medications that were stopped or started during admission. New medications that were started in the hospital to treat an acute condition may be continued by mistake at discharge.
Post-hospital discharge
The patient care team may not be informed of therapy changes that were made during the patient's hospital stay, and the patient may take medications that are no longer needed or miss medications that are critical to their treatment.
With healthcare moving more toward a value-based model, stakeholders have looked for innovative solutions to improve health outcomes and decrease costs. With the staggering costs associated with them, medication-related problems present a monumental opportunity.
How can medication-related problems be prevented?: Solve the problem before it happens
The good news is that the health and economic costs of MRPs are entirely preventable. Armed with cutting-edge technology and tools, care teams can stop medication-related problems before they happen.
Seeing the Future before it Happens: Data Science
Health plans and providers collect mountains of data every day that can be used to identify drug interactions and adverse drug effects early. Arine’s platform ingests and analyzes data from multiple sources including electronic medical records, prescription, and medical claims data, costs data, quality data, social determinants of health data, and digital device data. The platform analyzes this data and creates comprehensive data insights to help care teams intervene proactively and efficiently to prevent medication-related problems.
For example, one older patient had a history of frequent hospital admissions and diagnoses of CHF, COPD, and chest pain. He had not seen his primary care physician recently. Arine analyzed multidimensional data to identify that the patient was at risk for a medication-related problem and created a personalized care plan to help him get on the right medications. As a result, his clinical team optimized his CHF medications, triaged him to a smoking cessation program, and connected him to transportation to his physician. During the follow-up year, the patient stayed out of the hospital.
Turning information into action: automation, machine learning, and predictive analytics
Care teams can also leverage automation, machine learning, and predictive analytics to prevent MRPs.
Automation
AI-driven technology can connect and synthesize all of a patient’s data and automate manual work for the care team, such as automatically creating care plans, generating patient and provider communication letters, and assigning tasks to the appropriate person on the care team.
Predictive Analytics
Adding predictive analytics to the care team’s tool chest can help identify when high-risk, high-cost events will occur and enable care teams to get the right care to the right patient at the right time.
Machine Learning
Technology that learns from the result of every care team intervention can give health plans and providers the insight they need to understand what works and what doesn’t for their population and continuously optimize their care delivery.
Synthesizing multidimensional data into action
Technology that automatically integrates the whole patient picture of social, behavioral, and clinical risk factors along with evidence-based guidelines can help improve appropriate drug selection, address overprescribing or underprescribing, optimize medication doses, and decrease therapeutic inertia.
For instance, Arine’s AI-powered medication intelligence platform integrates current clinical practice guidelines into its algorithms to create evidence-based care plans and automatically generate patients' education and physician recommendations considering the unique patient needs. Care teams using the platform have all the information they need at their fingertips and can spend less time searching for guidelines to apply to patient care and more time counseling patients. Integration of guidelines also improves the standard of care, allowing clinicians to deliver the same high level of care as a clinician with years of experience.
Stopping medication-related problems once and for all
Healthcare providers and payers can come together to prevent medication-related problems. When you equip your care teams with the right tools, they can quickly scale care that prevents medication-related problems before they happen.
Register for our on-demand webinar to see how Arine incorporates AI to deliver comprehensive medication management and reduce medication-related problems:
Tags:
Blog PostsMay 5, 2022





Comments